AI-Powered Retinal Implant Restores Reading Ability for 84% of Blind Patients in New Trial

Image Credit: Christian Lue | Splash
A wireless retinal implant powered by artificial intelligence has enabled dozens of elderly patients blinded by advanced macular degeneration to read letters and words again, marking a milestone in bionic vision restoration, researchers reported on Sunday.
The device, known as PRIMA, combines a 2 millimetre square chip inserted beneath the retina with augmented reality glasses and a pocket processor that uses AI to process visual data into brain interpretable signals. Results from a multinational clinical trial, published in the New England Journal of Medicine, showed 84 percent of participants recovered enough central vision to read letters, numbers, and words, while 81 percent achieved at least two extra lines on standard acuity charts for an average uplift of five lines, with one reaching 12 lines. The trial targeted the dry form of age related macular degeneration, a condition affecting around 5 million people worldwide with irreversible central blindness from geographic atrophy.
Roots in Decades of Neural Engineering
Efforts to combat sight loss from macular degeneration trace back to the early 2000s, when Stanford ophthalmology professor Daniel Palanker began exploring light based neural stimulation during work on eye lasers. At the time, existing prosthetics offered only basic light perception, failing to deliver the form vision needed for practical use. Palanker's concept drew on the eye's natural transparency to beam information directly to surviving retinal cells, bypassing dead photoreceptors in the macula, the retina's light sensitive core.
This approach gained traction through collaborations with institutions like the University of Pittsburgh and the University of Bonn, culminating in PRIMA's development by Science Corporation, a firm specialising in brain computer interfaces. The technology addresses a gap in dry macular degeneration treatment, where slow cell death erodes central sight while sparing peripheral vision, forcing patients to rely on crude head movements for navigation. There are no approved therapies that restore lost central vision in dry AMD. In the U.S., two drugs (pegcetacoplan and avacincaptad pegol) are approved to slow geographic atrophy progression; in Europe, these were not approved as of 2025.
How AI Drives the Implant's Vision Processing
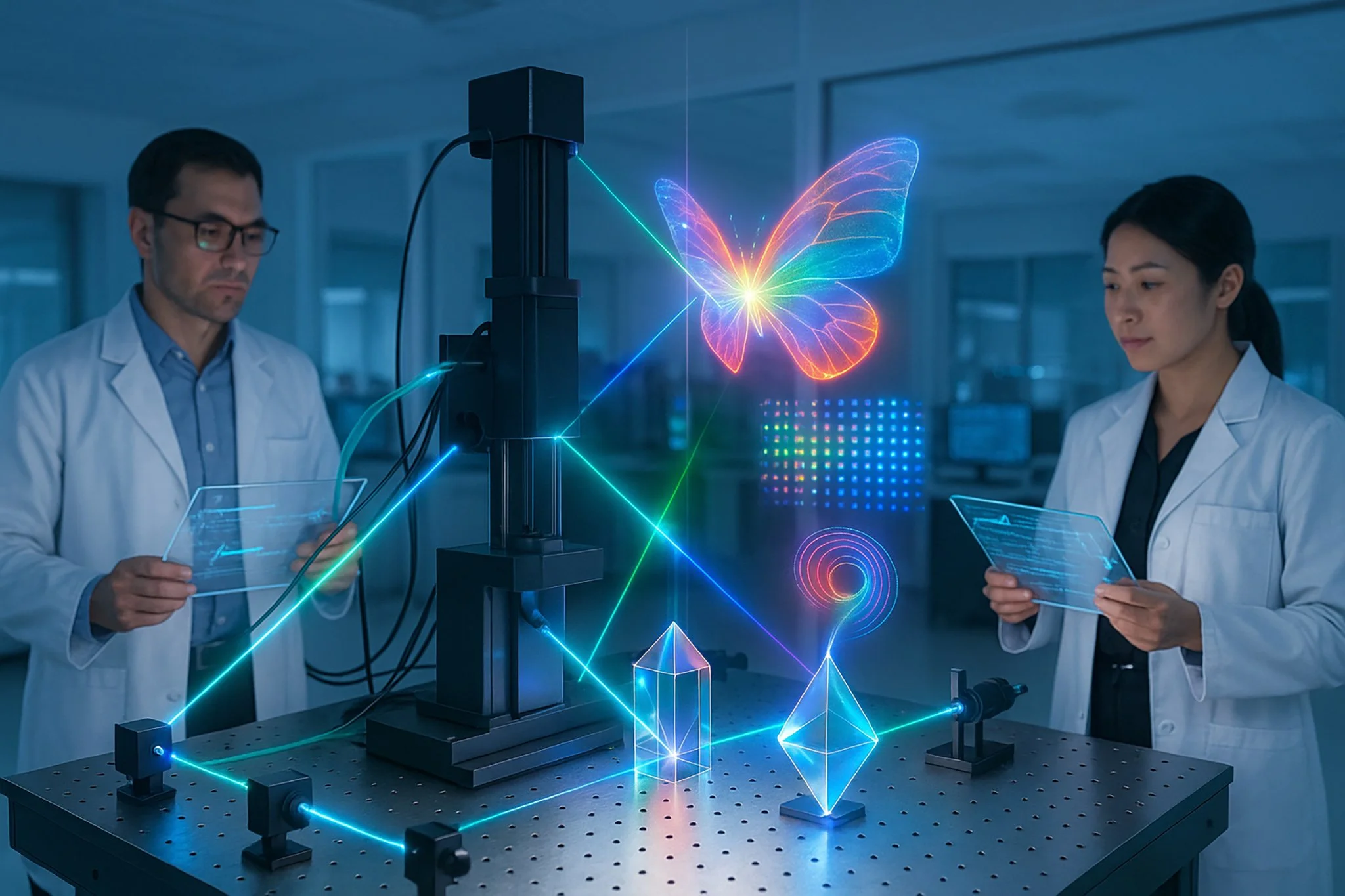
At PRIMA's heart sits a 2 millimetre square photovoltaic chip, just 30 micrometres thick, thinner than a human hair, implanted via a routine two hour vitrectomy surgery. The procedure removes the eye's gel like vitreous and slips the chip under the central retina through a tiny trapdoor incision, a task performed by vitreoretinal surgeons at specialist centres.
Once healed, patients don AR glasses fitted with a forward facing camera linked to a pocket processor. The camera feeds live scenes into AI algorithms that analyse and simplify images, projecting them as near infrared beams onto the chip's 378 pixels. Each pixel converts the light into electrical pulses, mimicking natural photoreceptor signals to activate underlying neurons and relay data via the optic nerve to the brain.
This AI layer proves crucial: it handles edge detection, contrast boosting, and up to 12 times magnification, tailoring output to individual needs without overwhelming the low resolution grid. Early versions yield black and white views, but software updates aim to introduce grayscale for finer details like facial outlines. The system's wireless design eliminates batteries or wires, allowing seamless integration with a patient's remaining peripheral sight for fuller spatial awareness.
Trial Outcomes Highlight Steady Gains
The pivotal trial enrolled 38 patients over 60 across 17 European hospitals in the UK, France, Italy, the Netherlands, and Germany, with Moorfields Eye Hospital in London handling the British cohort. All had lost central vision to geographic atrophy, scoring worse than 20/320 acuity in the treated eye, equivalent to legal blindness for near tasks.
After 12 months, 32 participants completed assessments, revealing no peripheral vision loss, and side effects like temporary eye pressure or minor bleeds resolved quickly in most cases, underscoring the implant's safety profile. Rehabilitation formed a core element, with months of sessions teaching users to scan images and interpret signals, much like adapting to hearing aids. Success metrics focused on functional benchmarks: recognising single characters evolved into fluid paragraph reading, with tools like zoom aiding progression from large print to fine text.
Voices from the Frontline: A Patient's Journey
Sheila Irvine, a 70 something book lover from Wiltshire, England, captured the human side of the shift. Pre implant, her world narrowed to distorted shadows, "like two black discs" blotting central view, halting her passion for novels. Four weeks post surgery at Moorfields, activation brought tentative breakthroughs: first letters, then numbers, building to deciphering prescription fine print or tin labels.
"It is dead exciting to see letters again", Irvine said, though she stressed the effort involved. "The more hours I put in, the more I pick up". Her story echoes broader trial feedback, where two thirds rated satisfaction medium to high, citing renewed independence in hobbies and errands, from crosswords to metro navigation in Paris.
Experts Weigh In on Broader Ramifications
Moorfields consultant Mahi Muqit, who led the UK trial arm, called the results "remarkable", signalling a new chapter where AI fused implants deliver tangible central vision for the first time. "It is not just popping a chip in the eye and seeing again", he noted. "You learn to use this vision, and that restores confidence".
Independent analysts point to ripple effects on elder care, as macular degeneration strikes hardest among those over 50, the top blindness culprit in developed nations. By enabling self reliance in reading meds or menus, PRIMA could ease caregiver burdens and cut healthcare costs tied to isolation. Yet challenges linger: the need for specialised rehab and device costs, though scalable surgery hints at wider reach in public systems.
Charting Paths Ahead in Artificial Sight
Looking forward, developers eye refinements to push boundaries. Palanker envisions chips with 10,000 pixels at 20 micron scale, tested in animals, potentially yielding 20/80 base vision boosted to near normal with digital aids. Grayscale upgrades top the list, unlocking face recognition, a close second to reading on patient wishlists.
Regulatory nods could follow soon, paving commercial rollout, while expansions target retinitis pigmentosa or diabetic retinopathy. Broader trends suggest AI's role will deepen, blending wearables with neural tech for hybrid sight, though equitable access remains key to avoiding divides in global eye health. As one expert put it, this is "the first version", with iterations promising to redefine blindness not as total, but treatable.
We are a leading AI-focused digital news platform, combining AI-generated reporting with human editorial oversight. By aggregating and synthesizing the latest developments in AI — spanning innovation, technology, ethics, policy and business — we deliver timely, accurate and thought-provoking content.